SeDI – The Semantic PACS for Clinical Practice
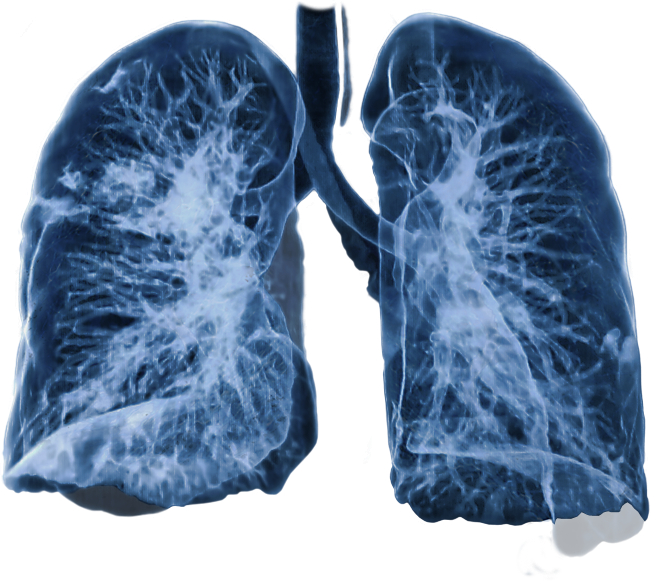
„Display all patients with a
bronchial carcinoma bigger than 50 cm³.“
Maybe you have wanted to create a similar search request for a PACS to consult comparable cases when making a diagnosis or to find matching cases for a clinical trial.
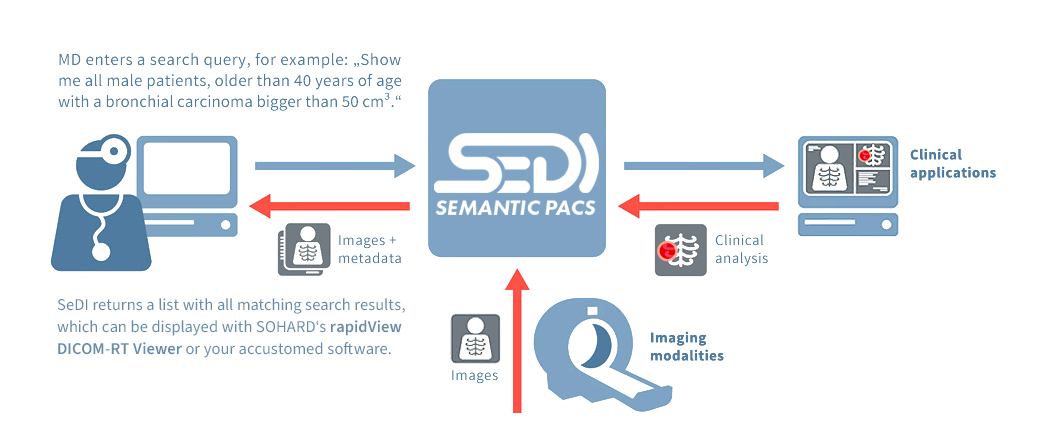
Conventional PACS are not capable of processing such requests. And although there are various powerful clinical applications to process image data and image data series to create significant clinical analyses, none of these analytic results can be merged with the clinical data of a single patient. However, retrieving this data is an essential prerequisite to perform such search queries.
SeDI is capable of answering such requests and providing the appropriate patient data. For the first time ever SeDI – as a semantic PACS – establishes the basis to search image data for specific attributes by integrating clinical data.
And as SeDI can query multiple attributes simultaneously, even complex searches are possible. In the example above, the query could be refined by more specific patient data like gender and age. With SeDI, you can easily find and access exactly the information you need – quickly and reliably.
How does SeDI work?
Supportive in clinical workflows and scientific research
With SeDI you can search the image and data pool of your PACS for reference cases, in order to confirm a suspected diagnosis or to optimize your patient’s treatments plans.
SeDI can also enable an automatic transfer of patient data from clinical IT systems to scientific IT systems. In this way SeDI can support you in your scientific research.
Using SeDI medical physics researchers at the Antoni van Leeuwenhoek/Netherlands Cancer Institute are now able to create a semantic database of all radiotherapy related DICOM metadata that can be quickly searched with the standard query language SPARQL using terms from DICOM and radiation oncology vocabulary. SeDI will enable the researchers from the radiotherapy department to rapidly find the right DICOM objects for analysis, as well as accelerate ongoing research in outcome prediction, toxicity modelling and radiomics – areas of research that are essential to Rapid Learning and clinical decision support in radiation oncology.
SeDI can assist you in your work, save valuable time and help you to increase the quality of your diagnoses and therapies, benefiting both you and your patients.
Significant benefits for radiotherapy
SeDI is developed under constant guidance of physicians and clinical experts to guarantee a high level of quality and practical relevance. The MAASTRO clinic in Maastricht (Netherlands), one of Europe’s leading centers for radiotherapy, is a close clinical cooperation partner in SeDI’s development. With good reason: SeDI holds enormous benefit for radiotherapy treatment. By implementing DICOM-RT objects, SeDI is able to output contourings, treatment plans and doses of radiation from referential cases.
And in combination with the webbased DICOM-RT-Viewer from SOHARD Software the data output can be displayed in a quick and comfortable manner.
As a result, radiation physicists and therapists have fast and easy access to comparable values and benchmarks to guide them in radiation planning and in important treatment decisions.
 „Thanks to SeDI the search process for specific patient data on a PACS has become a lot easier. We use SeDI together with our Medical Image Analysis. This helps us to retrieve 3-D volume renderings, tumour volume and mean lung dose calculations of previous cases in a fast and convenient way, together with the proper images and patient data. The availability of this important information helps us to make more accurate clinical decisions for cancer patients.“
„Thanks to SeDI the search process for specific patient data on a PACS has become a lot easier. We use SeDI together with our Medical Image Analysis. This helps us to retrieve 3-D volume renderings, tumour volume and mean lung dose calculations of previous cases in a fast and convenient way, together with the proper images and patient data. The availability of this important information helps us to make more accurate clinical decisions for cancer patients.“ 
Prof. Andre Dekker, MAASTRO Clinic, NL
SeDI can support you and your team in many other useful ways.
Please tell us about your requirements.
.
Your benefits at a glance
Quality Assurance
Easy accessible reference cases can help to revise and verify tentative diagnosis
Efficient in time and expenses
Saves precious time using an efficient searching process that displays results more quickly than ever before
Quality Enhancement
Easy accessible reference cases can also help to accelerate, complement and refine diagnosis and treatment planning
Huge benefits for radiotherapy
Facilitates clinical decision-making by displaying therapeutic margins, treatment plans and doses of radiation of referential cases
Easy integration into your IT environment
Compatible with any common PACS, accessible via established clinical applications
Huge benefits for scientific research
Simple search for case studies and targeted selection of cohorts for clinical research